Incidence of osteoarthritis (OA) has increased by 9% in the last 28 years. Prevalence of OA is reported to be 16.1% and it is more common in low- and middle-income countries. It has been reported that 240 million individuals worldwide have symptomatic OA and this rate is especially higher in women over the age of 60. Knee joint OA was detected in 654.1 million people over the age of 40 in 2022 and its incidence was reported to be 203 per 10 thousand people.

The prevalence of OA is 5.343 per 100 thousand individuals and its incidence is 430.4 per 100 thousand individuals in the Middle East and North African countries. In a study conducted in Europe, it was emphasized that OA-related drug use was 46.9% and that patients with pain were disconnected from work life, which brought a burden to the healthcare system. In a study conducted on very elderly individuals in the Ural-Altay region, it was stated that the prevalence was 27.7% and 13.8% of the patients were using medication.
As society ages and quality life expectancy increases, OA has begun to impose a threat on the quality of life of patients causing social and psychological disturbances. In a study conducted in 2014, it was stated that OA is expected to increase from 26.6% to 29.5% in individuals over the age of 45 in 2032. Knee involvement in OA is seen in 85% of patients. The European OA report published in 2022 emphasizes that the direct cost of the disease reached 7.2 billion Euros and the indirect cost reached 4.4 billion Euros.
Table 1. Common characteristics of OA
| A cyclical disease with multiple phenotypes, multiple etiologies, heterogeneous and low inflammatory. |
| Advanced age, female gender, black race, heredity, increased body mass index, trauma, inactivity. |
| Morbidity and mortality. |
| Meniscus tear, intra-articular or periarticular fracture and ligament injury or joint dislocation in secondary OA. |
| The symptoms are cyclically progressing pain, swelling, limitation of movement and deformity. |
| Decrease in the thickness of the articular cartilage, deterioration of its molecular structure and change in its microarchitecture: change in chondroitin-keratan sulfate ratios: chondro-senescence. |
| Degeneration (catabolic degradation) through the cycle of fibrillation, destruction and regeneration (anabolic construction) in articular joint cartilage. |
| Thinning and sclerosis on the articular surface. |
| Subchondral cyst formation and painful osteophytes with inflammation in the subchondral bone. |
| Thickening of the joint capsule, synovitis and decrease in joint fluid: changes in metabolites. |
| Meniscus degeneration and displacement from the joint space. |
| Skeletal muscle atrophy: sarcopenia. |
| Wearing of tendons and ligaments: deterioration of balance due to laxity and increased risk of falling. |
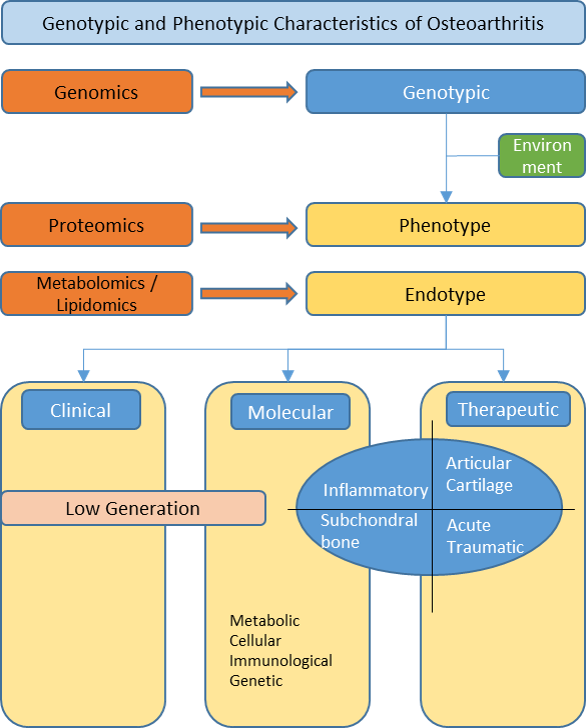
Figure 1. Intersection regions of omics analyzes with genotypic and phenotypic features of OA.
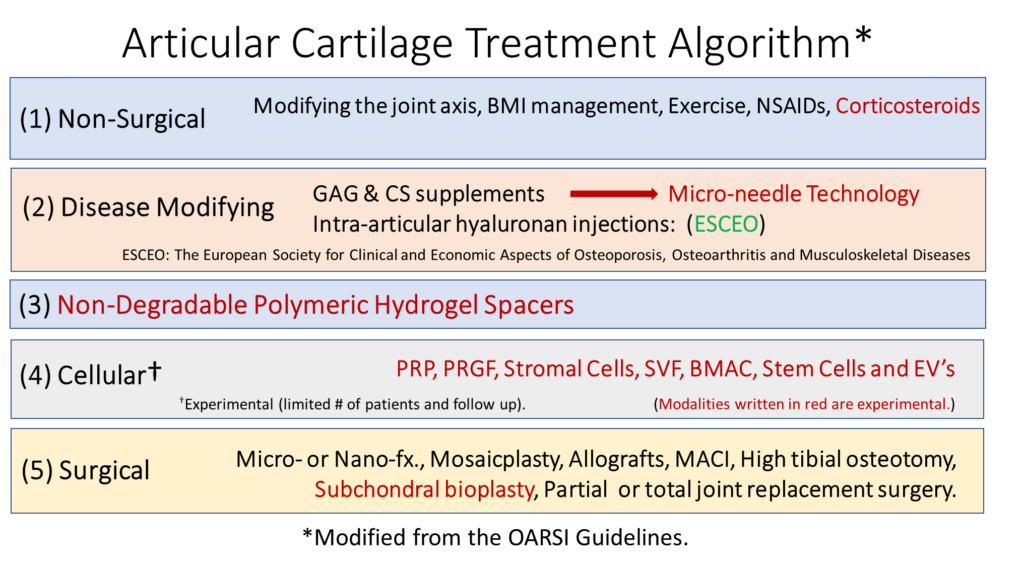
Figure 2. Knee OA Treatment Algorithm
Table 2. Synovial Joint Fluid Features
| Specification | Normal | Non-inflammatory | Inflammatory | Septic |
| Colour | Clear | Yellow | Yellow, opalescent | Yellow – Green |
| Clarity | Transparent | Transparent | Translucent-opaque | Opaque |
| Viscosity | High | High | Low | Variable |
| WBC/mm3 | 200 | 200-2000 | 2000-10.000 | >50.000 |
| Polymorphonuclear leukocytes (PMNs) | <25% | ~25% | >50% | >75% |
| Culture | Negative | Negative | Negative | Often positive |
| Glucose (mg/dL) | Nearly = to plasma | Nearly = to plasma | ~25, lower than plasma | <25, even lower than plasma |
Table 3. Joint Cartilage Biomarkers Classified According to Their Molecular Properties
| Formation Biomarkers: PIICP, PIIANP, PIIBNP, CPII, IGF-1, FGF, HA, Coll 2 |
| Degradation Biomarkers: CTX-II, C2C, CIIM, HELIX-II, Coll 2-1 NO2, COMP, CS846, Aggrecan Epitopes (ARGS, TEGE, FFGV), Fibulin-3 Epitopes (Fib3- 1, Fib3-2, Fib3-3), TIINE, Gly-Gal-Pyd, MMP2, MMP3, MMP9, MMP13, TIMP-2, TIMP-3, TIMP-4, ADAMTS-4, ADAMTS-5 |
| Inflammatory Biomarkers: IL-1 β, IL-1Ra, TNF, TNF-Rs, IL-2, IL-4, IL-6, IL-8, IL-10, IL-15, IL-17, IL-18, CXCL-10, PGE2, IL-8/CXCL-8, GROa/CXCL-1, MCP-1/CCL-2, RANTES/CCL-5, MIP-1α/CCL-3, MIP-1β/CCL-4, CCL2, CCL3, CCL, CCL5, CCL7, CCL21, VEGF, 15-HETE, CRP, CRPM, Resistin, Leptin, Adioponektin, ApoA1, MPO |
| PIICP: Procollagen II C-Terminal ProPeptide, PIIANP: Type IIA Collagen N-Propeptide, PIIBNP: The type II collagen N-propeptide, CPII: Type II collagen propeptide, IGF-1: Insulin-like growth factor-1, FGF: Fibroblast growth factors, HA: Hyaluronic acid, Coll 2: Collagen type II, CTX-II: Crosslinked C-telopeptides of type II collagen, C2C: Neoepitope of type II collagen, CIIM: Matrix metalloproteinase-derived fragment of type II collagen, HELIX-II: Helical peptide of type II collagen, Coll 2-1 NO2: Nitrated form of triple helical region of type II collagen, COMP: Cartilage oligomeric matrix protein, CS846: Chondroitin sulfate 846 epitope, TIINE: Type II collagen neoepitope, Gly-Gal-Pyd: Glucosyl-galactosyl-pyridinoline, MMP: Matrix metalloproteinase, TIMP: Tissue inhibitor of metalloprotease, ADAMTS: A disintegrin and metalloproteinase with thrombospondin motifs, IL: Interleukin, CXCL-10: CXC motif chemokine ligand, PGE2: Prostaglandin E2, GROa: Growth-regulated oncogene-alpha, MCP-1: Monocyte Chemoattractant Protein-1, CCL: The chemokine (C-C motif) ligand, RANTES: Raised on activation normal T-cell derived and secreted, MIP: Macrophage inhibitory protein, VEGF: Vascular endothelial growth factor, 15-HETE: 15-Hydroxy-eicosatetraenoic acid, CRP: C-reactive protein, CRPM: C-reactive protein metabolite, ApoA1: Apolipoprotein, MPO: myeloperoxidase |
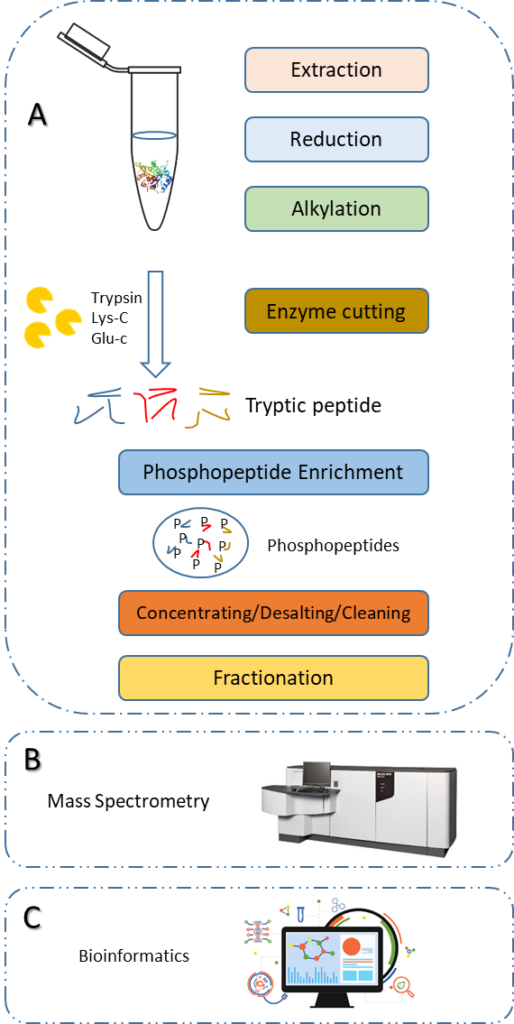
Figure 3. Schematic Representation of Phosphoproteomic Analysis Workflow
For Further Information
https://www.who.int/news-room/fact-sheets/detail/osteoarthritis